Endometriosis affects up to 10% of those who are menstruating
Under diagnosis, misdiagnosis and given the fact that it can take up to 5-10 years to receive a diagnosis, it’s hard to know the true prevalence of endometriosis.
Endometriosis is a condition where tissue to the endometrium (uterine lining) grow in  places other than the inside of the uterus and can result in severe period pain.
places other than the inside of the uterus and can result in severe period pain.
Abnormal growth can occur in areas in the pelvis, such as the ovaries, fallopian tubes and any tissue that lines the abdominal cavity.
The pain is generally more severe than cramping that can happen before your period.
It’s common the experience period-related symptoms, endometriosis is a “whole body inflammatory disease”. It’s a condition related to immune-system dysfunction.
Common endometriosis symptoms are:
- Severe period pain
- Heavy menstrual bleeding
- Pelvic pain
- Gut issues – diarrhea or constipation – or both
- Bladder problems – frequency, urgency, pain
- Abdominal bloating
- Nausea
- Headaches
- Fatigue
- Bleeding between periods
- Spotting before period
Overlapping with PMS symptoms can cause endometriosis to get written off as “normal” period symptoms. The reality is you should not have to be dealing with ANY symptoms – endometriosis or not!
Endometriosis is only diagnosed through laparoscopic surgery which is another huge problem. This is way more invasive than a blood test and may not be financially accessible and may not even be recommended depending on the level of your symptoms.
Ultrasound imaging can be difficult to assess superficial endometriosis but can be helpful for detecting endometriomas (blood-filled ovarian cysts) or deeply infiltrative endometriosis. Some blood tests can give insight into possible endometriosis.
So, what can be done with a kind of half diagnosis? You can still uncover the root causes of your symptoms and incorporate nutrition and lifestyle foundations to reduce pain, heavy periods and inflammation.
When I work with clients who-
- Have an endometriosis diagnosis
- Have suspected endometriosis
- Have symptoms of endometriosis but not yet diagnosed –
In each case we are looking at:
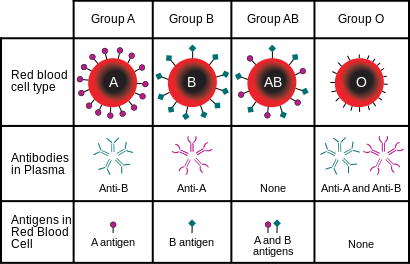
- Estrogen/Progesterone balance
- Estrogen metabolism – are you preferring the inflammatory 2-OH pathway or 16-OH pathway (here you can see more period pain/heavy bleeding)
- Are you ovulating?
- Gut health testing – gut issues are very common in those with endometriosis
- Cycle an symptom tracking – when in your cycle do your symptoms occur? What is your luteal phase length (need at least 10 days for progesterone production)?
- Inflammatory markers
- Nutrient deficiencies
- Exercise – movement is key for encouraging blood flow
- Stress (more stress more pain)
- Sleep
- Blood sugar balance
- Histamine response
- and of course more
Functional lab testing helps to assess estrogen and progesterone levels, possible estrogen dominance and looks at your estrogen metabolism – sometimes there is something going on with these hormones with endometriosis.
You can have estrogen dominance with normal estrogen levels and low progesterone or both could be in the normal range but estrogen is still high in relation to progesterone and could have poor estrogen metabolism which contributes to your symptoms.
Looking for some support?